Add your promotional text...
Patient Journey Through Hospital Billing Process to Insurance Companies
This document outlines the detailed workflow diagram that illustrates the patient journey through the hospital billing process to insurance companies. It provides a comprehensive view of the steps involved, from the moment a patient receives care to the final resolution of their billing with insurance providers. Understanding this journey is crucial for both healthcare professionals and patients to navigate the complexities of medical billing and insurance claims effectively.
Patient Receives Care: The journey begins when a patient receives medical services at the hospital.
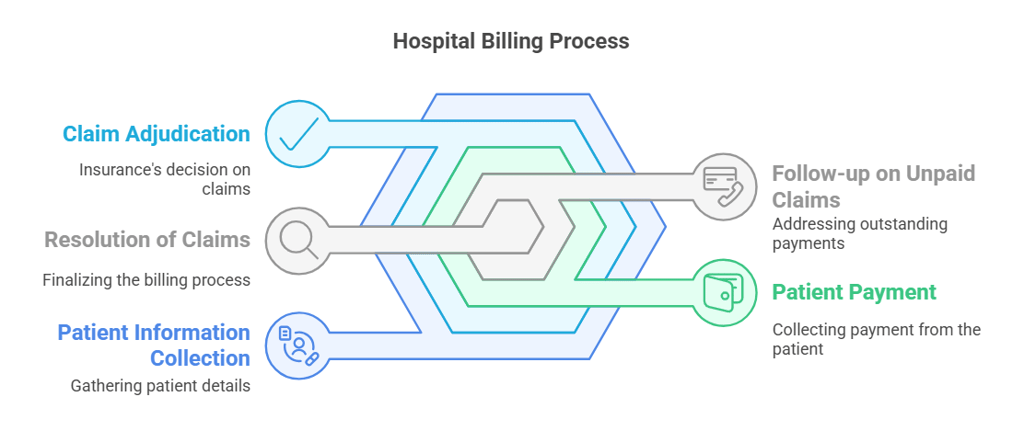
Patient Information Collection: The hospital collects necessary patient information, including personal details and insurance information.
Insurance Verification: The hospital verifies the patient's insurance coverage to ensure that the services provided are covered.
Service Coding: Medical coders assign codes to the services rendered based on the diagnosis and procedures performed.
Charge Entry: The coded services are entered into the hospital's billing system to generate charges.
Claim Submission to Insurance: The hospital submits a claim to the patient's insurance company for reimbursement.
Insurance Review: The insurance company reviews the claim to determine its validity and coverage.
Claim Adjudication: The insurance company adjudicates the claim, deciding how much will be paid to the hospital.
Payment Processing: The insurance company processes the payment based on the adjudicated claim.
Patient Billing Statement: After payment is received, the hospital generates a billing statement for the patient, detailing any remaining balance.
Patient Payment: The patient reviews the statement and makes payment for any outstanding balance.
Follow-up on Unpaid Claims: If there are unpaid claims, the hospital follows up with the insurance company for resolution.
Resolution of Claims: Finally, any outstanding issues are resolved, and the patient is informed of the final billing status.
This workflow diagram serves as a guide for understanding the intricate steps involved in the hospital billing process and the interactions with insurance companies, ensuring transparency and clarity for patients and healthcare providers alike.
Four Ways AI and Automation Improve Denial Management
AI and automation can significantly enhance denial prevention, management, and recovery through the following methods:
Preventing Denials: AI can analyze historical data to predict which claims are likely to be denied, allowing providers to address potential issues before submission.
Automating Routine Tasks: Automation can manage repetitive tasks like insurance verification and pre-authorization, minimizing human error and allowing staff to concentrate on more complex issues.
AI and automation can significantly enhance denial prevention, management, and recovery through the following methods:
Preventing Denials: AI can analyze historical data to predict which claims are likely to be denied, allowing providers to address potential issues before submission.
Automating Routine Tasks: Automation can manage repetitive tasks like insurance verification and pre-authorization, minimizing human error and allowing staff to concentrate on more complex issues.
Analyzing Denial Patterns: AI can identify common reasons for denials, enabling organizations to refine processes and training to reduce denial rates over time.saving time and increasing the likelihood of success.
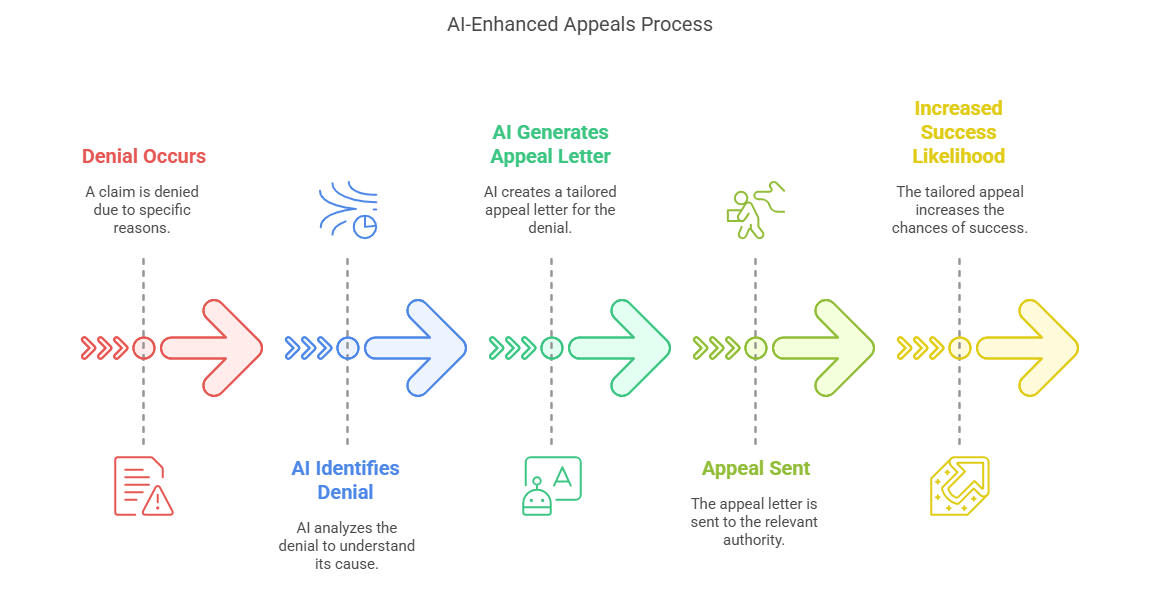
Streamlining Appeals: In cases of denial, AI can facilitate the appeals process by automatically generating appeal letters tailored to the specific reasons for denial.